Symptoms
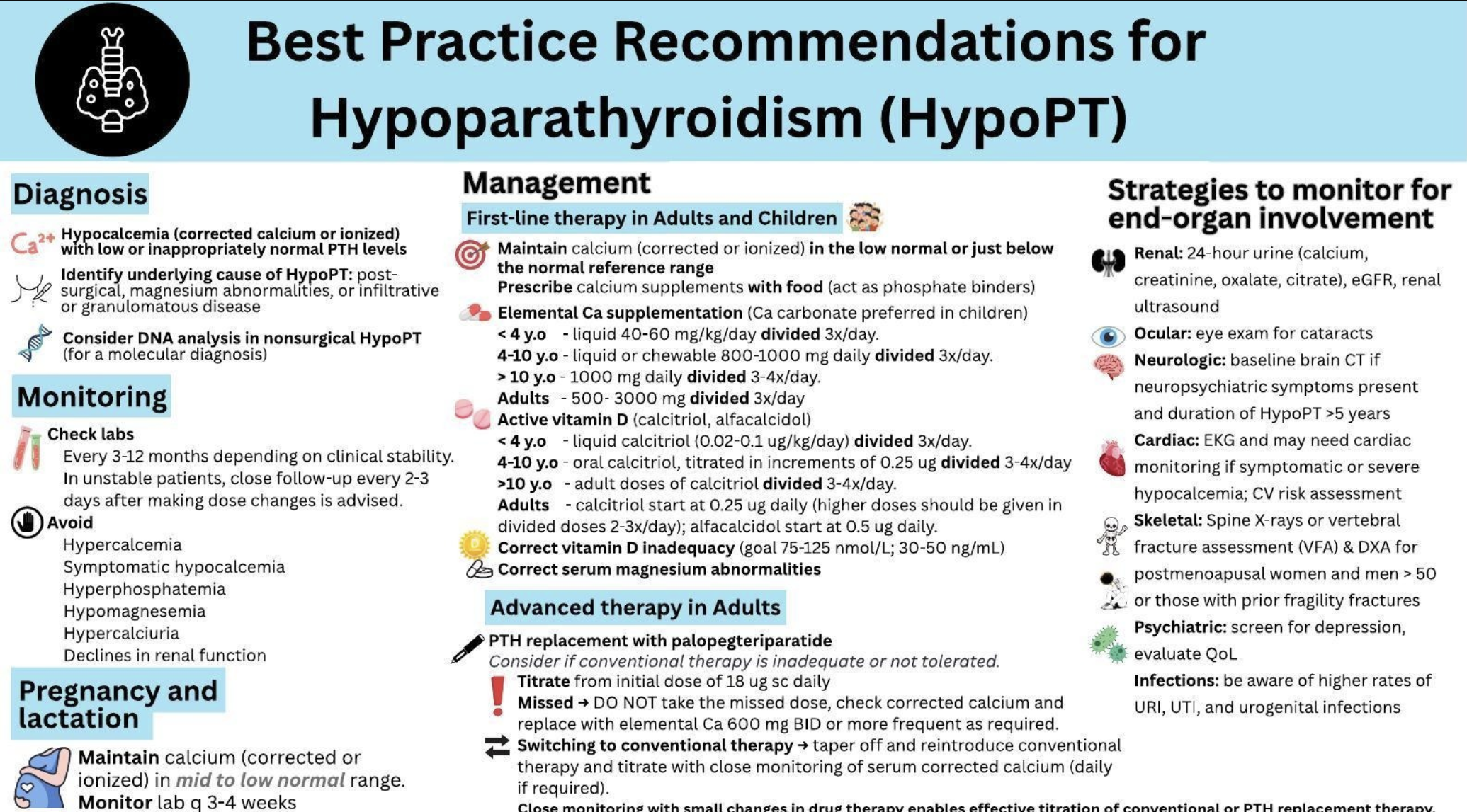
HypoPARAthyroidism is diagnosed when your blood calcium level is low AND your parathyroid hormone level (PTH) is low or absent at the same time.
There are a wide range of hypoPARAthyroidism symptoms and they can have numerous effects on the systems within the body, including the renal, cardiovascular, ophthalmological, and nervous systems.
Renal System
- Nephrocalcinosis – general deposits of calcium in the kidneys. May cause acute kidney injury
- Kidney Stones
- Chronic Kidney Disease
- Elevated Serum Phosphate level
Peripheral Nervous System
- Paraesthesia – a burning or prickling sensation sometimes referred to as numbness or tingling. Can also feel like skin crawling or itching
- Muscle Cramps
- Tetany – involuntary muscle contractions
Neuropsychiatric
- Cognitive dysfunction – deficits in attention, verbal and nonverbal learning, short term memory, problem solving, visual and auditory procession, processing speed may be slowed
- Poor quality of life
- Symptoms of anxiety and depression
- Poor memory
- Brain Fog
Central Nervous System
- Seizures
- Brain Calcifications – Calcium deposits in the brain, sometimes referred to as brain stones
- Parkinsonism or dystonia – neurological movement disorder, involuntary
Cardiovascular System
- Arrhythmias – irregular heartbeat
- Hypocalcemia associated dilated cardiomyopathy – heart chambers enlarge and lose ability to contract
Respiratory System
- Laryngospasm – temporary spasm of the vocal cords that makes it difficult to breathe or speak
- Bronchospasm or wheezing
Ophthalmological System
- Cataracts
- Papilledema – optic disc swelling caused by intracranial pressure
Dental System
- Altered tooth morphology
How is HypoPARA Treated?
Conventional Therapy for hypoPARAthyroidism consists of over-the-counter oral calcium supplements plus active forms of vitamin D, such as Calcitriol. Other medications and supplements may be used to treat symptoms of hypoPARA.
Follow the link to view the newly published guidelines
Guidelines PDF of Guidelines
Calcium Supplements and Calcitrol
Most doctors recommend using calcium citrate or calcium carbonate to treat low calcium levels. There are many brands of these forms of calcium available. Here are just a few:

Preparing for a calcium crash
It is important to discuss with your physician an emergency treatment plan. Many times when patients need to go to the emergency room for a calcium crash they can’t explain or remember what is needed and most emergency physicians don’t know how to treat our disease. Print this card and have your physician add information specific to your case. Then keep it in your wallet or purse for emergencies.
IMPORTANT NOTES*:
- Your body can’t absorb more than 500 mg at a time of calcium. Many of these brands only come in 600 mg doses. (Any amount over 500 mg in a dose goes to your kidneys and over time may cause kidney stones or nephrocalcinosis). If your physician prescribes more than 500 mg discuss with them spreading that dose out over the course of the day.
- It is generally not recommended to use TUMS as your source of daily calcium. Even though TUMS contains calcium carbonate it also contains other ingredients to block acid absorption in your stomach. Those ingredients are not meant to be taken long term as they may cause stomach issues, and they also can block calcium absorption as you need stomach acid to help absorb calcium.
- Also to be noted, calcium carbonate is harder on the stomach and not as easily tolerated by some.
Vitamin D
Your body also needs Vitamin D to help absorb the calcium. There are different forms of Vitamin D – Vitamin D2 and Vitamin D3. Calcitriol or Alphacalcidiol are the active form of Vitamin D3 (1,25-dihydroxycholecalciferlol ) and will help you absorb calcium and eliminate phosphorus. Some patients with hypoPARAthyroidism will also need to use Vitamin D2 or ergocalciferol. This helps maintain 25-hyrdroxyvitamin D (25(OH)D) levels.
Other Medications Sometimes Needed for HypoPARA
Magnesium
It is common for magnesium levels to be low when you have hypoPARAthyroidism. Magnesium also helps with absorption of calcium
Hydrochlorothiazide (HCTZ)
A diuretic is sometimes needed when your urine calcium levels become too high. This is given to protect the kidneys. Because HCTZ is not a potassium-sparing diuretic, you may also need to take a potassium supplement if you begin this medication.
Available Medications for HypoPARA Outside of the SOC
- Forteo (Teriparatide) - A PTH injection that is approved for Osteoporosis. This drug is considered off-label and is difficult to get covered by insurance.
- Yorvipath (Palopegteriparatide)- formerly known as Transcon PTH was approved by the FDA on Aug. 12th, 2024 and should be to market by Q1 of 2025
Drugs in Clinical Development for HypoPARA
- Eneboparatide – A once daily PTH injection
- Encalaret – A pill for ADH1 and ADH2. It works on the CaSR (calcium sensing receptor)
- MBX – A once weekly PTH injection
- Septerna - An oral PTHR1 agonist

Routine Monitoring
Routine monitoring and tests are performed to measure various blood levels, bodily function, and the progression of symptoms.
Every 3-12 Months
- Serum Calcium
- Magnesium
- eGFR
- Serum Creatinine
- Phosphate
- Serum Albumin Corrected Calcium Calculator
Every 6-24 Months
- 24-hour urine Calcium and Creatinine
- 25 OH(D)
Baseline Tests
Ophthalmologic exams are needed if a patient has visual symptoms. Renal imaging at baseline (e.g., ultrasound) is repeated subsequently if a patient has:
- Elevated urinary calcium greater than 400 mg per day and/or urine citrate is less than 300 mg per day renal calcification
- Stones
- Declining renal function
DXA, or bone density scans, are not needed routinely. BMD (bone mineral density) may not reflect bone strength accurately given most hypoPARA patients tend to have overly dense bones.
Clinical Trials & Research
Learn more about current available treatments for HypoPARA or for management of symptoms and types of doctors who treat HypoPARA.